
You are now leaving GSK’s website and are going to a website that is not operated/controlled by GSK. Though we feel it could be useful to you,we are not responsible for the content/service or availability of linked sites. You are therefore mindful of these risks and have decided to go ahead.
Agree StayThis page contains information for individuals aged SHINGLES 50 years and above.

Graphical representation only, not to scale.

Shingles, also known as herpes zoster, is caused by the reactivation of the varicella zoster virus. After experiencing chickenpox or exposure to the varicella zoster virus, the virus stays dormant in the body for life. With age, the immune system naturally weakens, which may allow the usually inactive virus to reactivate, causing Shingles.4
Hence, older people have an increased chance of getting Shingles. It typically produces a painful, blistering rash that appears on one side of the body or face.1,5

Shingles typically produces a painful and blistering rash, erupting in a stripe of blisters that wraps around either the left or right side of the torso, along a nerve path. It can develop on the torso, arms, thighs, or head (including in the eyes or ears).17 People often describe the pain as aching#, burning#, stabbing#, or shock-like#.2 It may interfere with everyday activities, like getting dressed, walking, and sleeping.2,20

A Shingles infection usually starts with a skin rash that affects a small part of the body. The affected person may also experience pain that feels like electric shocks# or piercing nails# or burns caused by boiling water#, itching, tingling, and numbness localised to the affected areas 48-72 hours before the rash appears.2,11
People can also experience fever, headache, chills or upset stomach.10
So, if you are experiencing any of these symptoms, please talk to a doctor quickly.
While most people recover from Shingles infection fully, some might face health complications
PHN (Postherpetic Neuralgia) is a health complication that affects up to 25% of people with Shingles. One of the main symptoms of PHN is nerve pain that continues for months or years after the Shingles rash is healed. The pain usually is experienced in the affected area.14
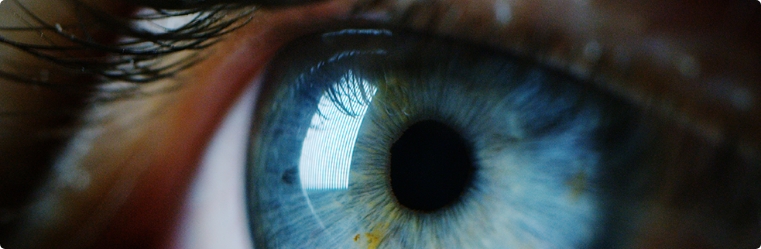
Ophthalmic complications occur in up to 50% of people with herpes zoster opthalmicus (HZO), a Shingles rash that involves the eye or nose. Up to 30% of people with HZO may develop double vision. Damage to the optic nerve of the eye is rare and occurs in less than 0.5% of people with HZO.13

Neurological complications such as encephalitis (swelling of the brain) are rare and estimated to occur in up to 1% of people who get Shingles.15
In rare cases, the Shingles virus can reactivate in the hearing system, leading to herpes zoster oticus. Symptoms include hearing impairment, vertigo, tinnitus, severe facial pain, and facial paralysis (Ramsay Hunt Syndrome). Problems with balance may develop in up to 1% of people with Shingles.16
This is not an exhaustive list of health complications arising after Shingles. Please speak to a doctor for more information.
The varicella zoster shingles virus is responsible for chickenpox. After a person has chickenpox, the virus stays in their body and becomes inactive. The virus can become active again years later and cause Shingles.4 Scientists aren’t exactly sure what causes the virus to become active again. However, there may be multiple factors. A person’s immune system weakens as they age.7 The more the immune system weakens, the less likely it is to prevent the virus from reactivating. Hence, older people are more at risk from Shingles.1,8
Firstly, anyone who has had chickenpox already has the virus that can cause herpes zoster disease. Some people have had chickenpox and don’t remember it or might not have realised it. Either way, they can develop Shingles disease symptoms if the virus reactivates, despite how healthy they may feel.4
People with low immunity are at a higher risk of developing Shingles.7 And since the immune system naturally weakens over time with age, people are at a higher risk after age 50.1,7
Older adults are also at increased risk of having complications such as Post-herpetic Neuralgia (PHN).5
The virus that causes Shingles is already present in the body from when you are infected with chickenpox. It goes dormant until reactivated.4 Hence, you cannot pass it on to another.
However, as Shingles is contagious it could infect another if they haven’t had chickenpox or aren’t protected against it. The virus could be transmitted if the person comes into direct contact with the blisters of someone with Shingles to develop chickenpox.9
Shingles typically produces a painful rash that often blisters, and scabs over in 10 to 15 days and clears up within 2 to 4 weeks. It usually appears on one side of the body or face.10 People with herpes zoster can have pain, itching, or tingling in the area where the rash will develop.11
There is a possibility that stress can increase your risk of Shingles.12 That said, age is the most important factor for developing Shingles. Most of the Shingles cases occur in adults 50 years and older.1
Please speak with your doctor to know more.
Chickenpox is a very contagious disease that causes a blister-like rash typically all over the body, itching, and fever. The chickenpox virus can reactivate, and become a reason for Shingles. People with Shingles may have pain, itching, tingling, and blisters in one area of the body that can last for weeks.4
Individuals who have never experienced chickenpox or have not received the chickenpox vaccine may contract the VZV virus from individuals with Shingles. This transmission can occur through direct contact with the fluid from Shingles rash blisters or by inhaling virus particles released from the blisters. In the event of infection, these individuals will manifest symptoms of chickenpox rather than Shingles symptoms and may potentially develop Shingles later in life.9
Herpes Zoster Ophthalmicus is a Shingles infection that affects the eye and the ocular area. Symptoms include forehead rash and painful inflammation of all the tissues.13
If you get Shingles, talk to your doctor to know more about Shingles and its prevention.
Shingles Prevention Options Shingles is caused by the reactivation of the virus that remains in the body after chickenpox. So, if a person hasn’t had chickenpox, ask them to avoid contact with people who have chickenpox or Shingles. Also, ensure that they follow all hand and cough hygiene to reduce the risk of developing chickenpox.4,9
Vaccination may help prevent Shingles.18 Talk to your doctor to know more about Shingles and its prevention.
Vaccination boosts your bodys immune system so it can fight off the Shingles virus and keep it from reactivating.18
Treatment may reduce the severity and duration of illness and depending on your symptoms may include weakening the virus and/or pain relief.
If you think you may have shingles, please speak with your doctor as soon as possible. They may prescribe appropriate medicines to help reduce the severity and duration of your symptoms.
General advice for managing symptoms:19
Speak to a doctor to know more about Shingles and its prevention.


Shingles in Lung Disease Patients: The Impact of Asthma and COPD

Shingles and Diabetes: Connection, Impact and Prevention

Autoimmune Diseases and Shingles: Understanding Their Connection and Impact

Shingles in Lung Disease Patients: The Impact of Asthma and COPD
‘Anti-shingles vax a must in preventive armour of adult vaccination’
Source : The Times of India Read more
GlaxoSmithKline and Amitabh Bachchan join forces to raise ‘Shingles’ awareness
Source : ET Brand Equity Read more
GSK to bring Herpes Zoster vaccine Shingrix at one-third of US price: MD
Source : Business Standard Read more